A Guide to Surgery
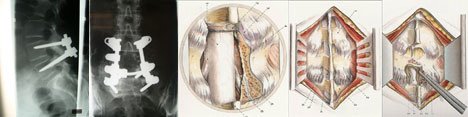
Anterior lumbar interbody fusion
The ALIF approach has the advantage that, both the back muscles and nerves remain undisturbed.
About the surgery
Anaesthesia: The surgery is usually performed under a general anaesthetic with the patient lying on the back.
Procedure: In the anterior lumbar interbody fusion (ALIF) approach, the disc space is fused by approaching the spine through the abdomen. A 7-10cm incision is made in the abdomen and the abdominal muscles are retracted to the side.
The anterior abdominal muscle in the midline (rectus abdominis), is retracted to the side. The abdominal contents lay inside a large sack (peritoneum) that can also be retracted, thus allowing the spine surgeon access to the front of the spine. The large blood vessels that continue to the legs (aorta and vena cava) lay on top of the spine, so your spine surgeon may perform this surgery in conjunction with a general surgeon who mobilizes the large blood vessels. After the blood vessels have been moved aside, the disc material is removed and a cage filled with bone morphogenic protein (BPM) is inserted. The incision is closed with dissolvable sutures and a drain tube removes the blood that collects at the surgical site.
After surgery
Following surgery, you will be transferred to the recovery room and may feel some pain at the operated site when you wake up. A patient controlled analgesia (PCA) pump will be provided which releases a small dose of pain medication every time you press the button, thereby putting you in control of your pain. You will be given intravenous fluids to keep you hydrated and a urinary catheter will empty your bladder. When the medical staff in the recovery room are confident that you are comfortable, you will be transferred to your room.
In the ward: Since the abdomen was opened during surgery, you will be advised not to eat or drink anything for the first 12 -24 hours. You will then be commenced on a clear fluid diet and gradually progress to a light diet. On the day after surgery, the drain tube, urinary catheter and pain pump will be removed and you will be encouraged to walk wearing a brace for support. You will stay in the hospital for 3-5 days and your surgeon will decide when you can go home.
Pain relief: Although we expect that you will be in pain or discomfort, we recommend that you take regular pain relief following surgery. Medications will be provided to reduce your pain after surgery and at home for the first 1-2 weeks. If pain persists after discharge please seek advice from Spine Service or your General Practitioner.
Skin sutures: Dissolvable sutures are most often used to close the skin. These will dissolve as your wound heals, however, the tip of the suture on either end of the incision will need to be cut on your first visit to the surgeon's office 7-10 days after surgery.
What to expect following surgery
Pain: You will feel discomfort and pain at the operative site immediately after surgery. You will be given pain medications; however, the soreness and stiffness in your back and/or limbs will continue for some time. Please ensure you take regular pain relief.
Tingling / Numbness: A degree of tingling and/or numbness in your limbs may be experienced after surgery and may take some time to subside.
Drains: Some patients may return to the ward with a drain tube near the surgical site to help prevent any collection of fluid at the operation site. The drain is usually removed in 24 to 48 hours.
Drips: You will have a small plastic needle (cannula) to receive fluids and antibiotics during and after surgery. The cannula will be removed when you are drinking sufficient fluids and after the doctor has stopped the prescribed antibiotics.
Catheter: A catheter will be inserted into your bladder under anaesthesia to drain you bladder during and immediately after surgery. This catheter will keep you comfortable, so you will not have to get out of bed to go to the toilet on the first day. The catheter is usually removed the day after surgery.
Calf compressors: Following your surgery, you will have inflatable compressors on your calves to reduce the risk of deep vein thrombosis (DVT). You may also be given a pair of anti-thrombotic stockings.
Coping with the Blues: It is not uncommon for patients to feel a little depressed or emotional after your surgery. The doctors and nurses will help you through this vulnerable phase.
Diet: You will be Nil by Mouth initially allowed only sips of fluid and crushed ice to suck. Once bowel sounds are present, you will start on a post-operative diet and gradually increase to a full diet. To avoid constipation, you should include plenty of roughage, cereals, fruit & vegetables in your diet. You should also aim to drink 2-3 litres of fluid daily.
Bowels: It is common not to have bowel movements for the first few days. Once you have started on a full diet, you will be given medications to help with bowel movements.
ALIF surgery potential risks and complications
All surgical procedures are associated with a risk of complications and all risks should be discussed with your surgeon. The risks may be associated with the anaesthesia given or the surgical procedure per se. Surgical complications can include bleeding, infection, spinal fluid leak, injury to the veins and arteries near the spine or injury to the spine's nerve tissue or its surrounding protective layer.
Injury to the spinal cord or the nerves may occur during surgery and can result in complete paralysis of all four limbs or paralysis of certain muscles in the arms or legs, with loss of normal sensation. Loss of bowel and bladder control can also occur following injury to the nerves. An injury to the covering layers of the nerves (dura) can result in a leak of spinal fluid and this may occasionally require a repeat surgery. Great care is taken to ensure the accurate placement of the screws, including the use of intra-operative fluoroscopy (x-rays).
Although antibiotics are given before and after surgery, there is a 1-5% incidence of wound infection. Superficial mild infections can be treated with antibiotics, while deep infections may require a wound wash-out under anaesthesia. If you have had an infection in any other region (urinary bladder, chest and skin) immediately prior to surgery, you may be at a higher risk of post-operative infection in the spine, so let your surgeon know.
Venous thrombosis (DVT: clotting of blood in your calf muscles) and pulmonary embolism are uncommon after an elective spine surgery, particularly when you are out of bed and walking within 24 hours after surgery. We use calf compressors and TED stockings to prevent the clotting of blood in legs; we do not routinely use medications. However, if you have had an episode of DVT in the past, let your surgeon know.
There is a major risk that is unique to the ALIF approach. The procedure is performed in close proximity to the large blood vessels that go to the legs. Damage to these large blood vessels may result in excessive blood loss. Quoted rates in the medical literature put this risk at 1% to 15%.
For males, another risk unique to this approach is that approaching the L5-S1 (lumbar segment 5 and sacral segment 1) disc space from the front has a risk of creating a condition known as retrograde ejaculation. There are very small nerves directly over the disc interspace that control a valve that causes the ejaculate to be expelled outward during intercourse. By dissecting over the disc space the nerves can stop working, and without this coordinating innervation to the valve, the ejaculate takes the path of least resistance, which is up into the bladder. The sensation of ejaculating is largely the same, but it makes conception very difficult (special harvesting techniques can be utilized). Fortunately, retrograde ejaculation happens in less than 1% of cases and tends to resolve over time (a few months to a year). This complication does not result in impotence as these nerves do not control erection.
In general, the principal risk of this type of spine surgery is that a solid fusion will not be obtained (nonunion) and further surgery to re-fuse the spine may be necessary.
Nonunion rates are higher for patients who have had prior lower back surgery, patients who smoke or are obese, patients who have multiple level fusion surgery, and for patients who have been treated with radiation for cancer. Not all patients who have a nonunion will need to have another fusion procedure. As long as the joint is stable, and the patient's symptoms are better, more back surgery is not necessary.
Other than nonunion, the risks of a spinal fusion surgery include infection or bleeding. These complications are fairly uncommon (approximately 1% to 3% occurrence). In addition, there is a risk of achieving a successful fusion, but the patient's pain does not subside.
There are certain warning signs you should look for after surgery that may indicate a problem, such as excessive bleeding, redness or discharge from the wound, fever, weakness or numbness of the legs, or problems urinating. If you notice any worrisome symptoms, notify your surgeon at once.
Commonly asked questions
Will I need a blood transfusion?
Although some blood loss occurs during surgery, a blood transfusion is not generally required. More extensive surgeries may occasionally require a blood transfusion.
How long will I stay in hospital?
The length of your stay in the hospital will depend on the surgical procedure that you have had and can vary from an overnight stay to a week. It will also depend on how your wound is healing. You will be given a rough idea regarding the length of your stay during the pre-surgical education session. However, your surgeon will make a final decision after the operation.
When can I walk?
You will usually be encouraged to begin walking the morning after surgery.
Do I have to wear a back/neck brace?
Yes, you will be required to wear your brace when sitting, standing and walking after surgery. Your physiotherapist will wean you off as appropriate.
When can I have a shower after my surgery?
You can have a shower the day after your surgery. If your dressing gets wet, a new one can be applied.
When do I see my doctor after my surgery?
During your pre-surgical education session, the clinical co-ordinator will make an advance appointment for you to visit the rooms after you have been discharged from the hospital. This date can be changed depending on the length of your hospital stay.
Do I have stitches to come out?
The wound is usually closed with dissolvable sutures under the skin and these do not need to be removed. Metallic staples or non-dissolvable sutures, if used, will need removal. On your first appointment (10 days post-op) the surgical wound will be examined and the sutures/staples will be removed.
Do I need to attend physiotherapy sessions?
Following surgery a physiotherapy programme will be started to retrain you to maintain good posture and teach you the correct way of moving your spine.
Is there a certain position that I should sleep in at night?
The most important thing is for you to be comfortable. Some people find it comfortable to sleep with a pillow between their legs or under their thighs.
When is it safe to engage in sexual relations?
This is a very personal domain and is left up to you; whenever you think that you and your partner are ready. Clinically, a two-week period is recommended, provided you are the less active partner.
How long should I wait before driving a car?
The recommendation is to wait 3-4 weeks before driving a car. This may vary depending on your surgery and your progression during rehabilitation.
When can I go back to work?
This is assessed on patient-to-patient bases. If you have a physical occupation, it may take up to 3-6 months. With a sedate occupation, you could be back at work as soon as 3 weeks. Do not commence work until you speak to your doctor and physiotherapist.
When is it safe to bend and/or lift items heavier than a bag of sugar?
During the post-surgical physiotherapy sessions, you will be taught the correct way to bend and lift. Bending from the hips is fine if carried out in a controlled manner, but avoid heavy lifting objects (more than 3kg) till your physiotherapy commences.
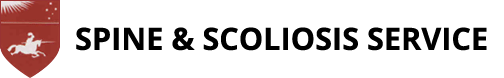
Anterior Cervical Decompression Fusion
 Anterior Cervical Spine Surgery
Anterior Cervical Spine Surgery
What is a disc prolapse?
This is also referred to as a slipped disc or disc herniation and usually occurs between the ages of 25-50 years. The jelly-like central portion of the disc (nucleus pulposus) tears through the surrounding layers (annulus pulposus) and is displaced into the spinal canal, compressing the nerves extending from the spinal cord.
Disc prolapse symptoms occur as a result of compression on the spinal cord or the nerves going to the arms. Pain in the arms that increases on coughing and sneezing is a symptom of disc herniation. Numbness, the sensation of pins and needles, and muscular weakness in the arms and hands may also be present. When the prolapsed disc compresses the spinal cord (myelopathy), it can cause difficulty in walking, clumsiness of the hands and problems with urinating. The presence and severity of these symptoms vary from person to person.
Who needs surgery?
Surgery is reserved for those with:
- No relief of pain with non-operative forms of treatment;
- Increasing numbness and weakness in the arms and hands; or
- The presence of myelopathy, which indicates the need for early surgery.
About the surgery
Anaesthesia: The surgery is usually performed under general anaesthesia, with the patient lying on the back.
Procedure: The surgeon makes a 2.5 to 5 cm incision in the skin in the front of the neck. The spine is exposed by retracting the muscles and blood vessels. The bulged disc is removed using special instruments and the pressure on the nerve roots and spinal cord is relieved. After the removal of the disc, the resultant gap is filled with a spacer (cage) made from a plastic material called PEEK and filled with an artificial bone graft substitute called VITOSS and OP-1. A titanium plate with screws is then used to fix the spine. A drain tube will remove the blood that collects at the surgical site. Skin sutures: Dissolvable sutures are used to close the skin. These will dissolve as your wound heals, however, the ends of the suture on either end of the incision will need to be cut on your first visit to the surgeon's office (7-10 days after surgery).
After the surgery
In the recovery room: Following surgery, you will be transferred to the recovery room and may feel some pain at the operated site when you wake up. A patient-controlled analgesia (PCA) pump will be provided, which releases a small dose of pain medication every time you press the button thereby putting you in control of your pain. You will be given intravenous fluids to keep you hydrated and a urinary catheter will empty your bladder. A neck collar will be provided to prevent excessive neck movements and to keep you comfortable. When the medical staff in the recovery room is confident that you are comfortable, you will be transferred to your room.
In the ward: You will be allowed to drink sips of fluids after surgery and gradually progress to a full diet. The day after surgery, the drain tube, urinary catheter and pain pump will be removed and you will be encouraged to walk wearing a brace to support your spine. You will stay in the hospital for 1-3 days and your surgeon will decide when you can go home.
Pain relief: Although we expect that you will be in pain or discomfort, we recommend that you take regular pain relief following surgery. Medications will be provided to reduce your pain after surgery and at home for the first 1-2 weeks. If pain persists after discharge please seek advice from Spine Service or your General Practitioner.
Skin sutures: Dissolvable sutures are most often used to close the skin. These will dissolve as your wound heals, however, the tip of the suture on either end of the incision will need to be cut on your first visit to the surgeon's office 7-10 days after surgery.
What to expect following surgery
Pain: You will feel discomfort and pain at the operative site immediately after surgery. You will be given pain medications; however, the soreness and stiffness in your back and/or limbs will continue for some time. Please ensure you take regular pain relief.
Tingling / Numbness: A degree of tingling and/or numbness in your limbs may be experienced after surgery and may take some time to subside.
Drains: Some patients may return to the ward with a drain tube near the surgical site to help prevent any collection of fluid at the operation site. The drain is usually removed in 24 to 48 hours.
Drips: You will have a small plastic needle (cannula) to receive fluids and antibiotics during and after surgery. The cannula will be removed when you are drinking sufficient fluids and after the doctor has stopped the prescribed antibiotics.
Catheter: A catheter will be inserted into your bladder under anaesthesia to drain you bladder during and immediately after surgery. This catheter will keep you comfortable, so you will not have to get out of bed to go to the toilet on the first day. The catheter is usually removed the day after surgery.
Calf compressors: Following your surgery, you will have inflatable compressors on your calves to reduce the risk of deep vein thrombosis (DVT). You may also be given a pair of anti-thrombotic stockings.
Coping with the Blues: It is not uncommon for patients to feel a little depressed or emotional after your surgery. The doctors and nurses will help you through this vulnerable phase.
Diet: You will be Nil by Mouth initially allowed only sips of fluid and crushed ice to suck. Once bowel sounds are present, you will start on a post-operative diet and gradually increase to a full diet. To avoid constipation, you should include plenty of roughage, cereals, fruit & vegetables in your diet. You should also aim to drink 2-3 litres of fluid daily.
Bowels: It is common not to have bowel movements for the first few days. Once you have started on a full diet, you will be given medications to help with bowel movements.
Are there any risks involved in disc surgery?
All surgical procedures are associated with a risk of complications and all risks should be discussed with your surgeon. The risks may be associated with the anaesthesia given or the surgical procedure per se. Surgical complications can include bleeding, infection, spinal fluid leak, injury to the veins and arteries near the spine or injury to the spine's nerve tissue or its surrounding protective layer.
Injury to the spinal cord or the nerves may occur during surgery and can result in complete paralysis of all four limbs or paralysis of certain muscles in the arms or legs, with loss of normal sensation. Loss of bowel and bladder control can also occur following injury to the nerves. An injury to the covering layers of the nerves (dura) can result in a leak of spinal fluid and this may occasionally require a repeat surgery. Great care is taken to ensure the accurate placement of the screws, including the use of intra-operative fluoroscopy (x-rays).
Although antibiotics are given before and after surgery, there is a 1-5% incidence of wound infection. Superficial mild infections can be treated with antibiotics, while deep infections may require a wound wash-out under anaesthesia. If you have had an infection in any other region (urinary bladder, chest and skin) immediately prior to surgery, you may be at a higher risk of post-operative infection in the spine, so let your surgeon know.
Venous thrombosis (DVT: clotting of blood in your calf muscles) and pulmonary embolism are uncommon after an elective spine surgery, particularly when you are out of bed and walking within 24 hours after surgery. We use calf compressors and TED stockings to prevent the clotting of blood in legs; we do not routinely use medications. However, if you have had an episode of DVT in the past, let your surgeon know.
There are certain warning signs you should look for after surgery that may indicate a problem, such as excessive bleeding, redness or discharge from the wound, fever, weakness or numbness of the legs, or problems urinating. If you notice any worrisome symptoms, notify your surgeon at once.
Talk to your surgeon
This is a brief overview and does not include all the known facts about your condition and the surgery. Feel free to seek any clarifications from your surgeon and his or her team. It is important for you to obtain a clear understanding of your condition, the surgery and the potential risks and benefits before you sign the consent form.
Lumbar Disc Replacement
Anatomy of the spine
The spine consists of 33 bony blocks called vertebrae stacked one above the other with a soft intervertebral disc between each pair of vertebrae. The intervertebral disc consists of a soft jelly-like substance called the nucleus pulposus in the centre, which is surrounded by multiple layers of collagen called the annulus fibrosis (like an onion). The disc connects and allows movement between the vertebrae and acts as a shock absorber for the spine. The vertebrae surround and protect the spinal cord and nerve roots.
The neck, also called the cervical spine, consists of seven vertebrae with an intervertebral disc in-between each pair of vertebrae.
Who needs a posterior cervical (neck) spine surgery?
- When the problem causing symptoms is located in the posterior aspect of the spine;
- when the compression on the spinal cord is from the posterior aspect;
- when the cervical spine is excessively mobile and unstable; or
- in association with an anterior procedure to provide additional stability or to achieve additional decompression.
The compression can be on the nerves going to the arms or on the spinal cord. Compression of the nerves in the neck can cause pain radiating down the arm and forearm with numbness, pins and needles, and muscular weakness in the affected limb. When the compression is on the spinal cord (myelopathy), it can cause difficulty in walking, clumsiness of the hands and problems with passing urine. The presence and severity of these symptoms vary from person to person. Pain in the neck could arise from numerous structures. Degeneration of the intervertebral disc and arthritis of the facet joints are the common causes of neck pain.
Who needs surgery?
Surgery is reserved for those with:
- No relief of pain with the non-operative forms of treatment;
- Increasing numbness and weakness in the arms and hands;
- Or the presence of myelopathy indicates the need for early surgery.
After assessing your symptoms, examining your spine, and studying your x-rays and scans, the surgeon will decide whether you need a posterior spinal decompression, a spinal fusion or a combination of both.
About the surgery
Anaesthesia: The surgery is usually performed under general anaesthesia, with the patient lying on the tummy. Occasionally, a frame is attached to the skull after anaesthesia, to maintain the position of the head during surgery.
Procedure: The surgeon makes a 5-15cm incision in the skin on the back of the neck. The spine is exposed by retracting the muscles. Depending on the plan, a decompression, a fusion or a combination of both is performed. A decompression is performed by removing one or more bony laminae and any other structure overlying the spinal cord. A fusion is performed by inserting screws into the bones over the back of the spine and connecting the screws with rods. Occasionally, a combination of a decompression and a fusion is performed. At the end of the surgery a drain tube is inserted to remove the blood that collects at the surgical site.
Skin sutures: Dissolvable sutures are used to close the skin. These will dissolve as your wound heals, however, the ends of the suture on either end of the incision will need to be cut on your first visit to the surgeon's office (7-10 days after surgery).
After the surgery
In the recovery room: Following surgery, you will be transferred to the recovery room and may feel some pain at the operated site when you wake up. A patient controlled analgesia (PCA) pump will be provided, which releases a small dose of pain medication every time you press the button thereby putting you in control of your pain. You will be given intravenous fluids to keep you hydrated and a urinary catheter will empty your bladder. A neck collar will be provided to prevent excessive neck movements and to keep you comfortable. When the medical staff in the recovery room is confident that you are comfortable, you will be transferred to your room.
In the ward: You will be allowed to drink sips of fluids after surgery and gradually progress to a full diet. The day after surgery, the drain tube, urinary catheter and pain pump will be removed and you will be encouraged to walk wearing a brace to support your spine. You will stay in the hospital for 1-3 days and your surgeon will decide when you can go home safely.
Are there any risks involved in disc surgery?
All surgical procedures are associated with a risk of complications and all risks should be discussed with your surgeon. The risks may be associated with the anaesthesia given or the surgical procedure. Surgical complications can include bleeding, infection, spinal fluid leak, injury to the veins and arteries near the spine or injury to the nerve tissue of the spine or its surrounding protective layer
Injury to the spinal cord or the nerves may occur during surgery and can result in complete paralysis of all four limbs or paralysis of certain muscles in the arms or legs with loss of normal sensation. Loss of bowel and bladder control can also occur following injury to the nerves. An injury to the covering layers of the nerves (dura) can result in a leak of spinal fluid and this may occasionally require a repeat surgery. Great care is taken to ensure the accurate placement of the screws including the use of intra-operative fluoroscopy (x-rays).
Although antibiotics are given before and after surgery, there is a 1-5% incidence of wound infection. Superficial mild infections can be treated with antibiotics, while deep infections may require a wound wash-out under anaesthesia. If you have had an infection in any other region (urinary bladder, chest and skin) immediately prior to surgery, you may be at a higher risk of post-operative infection in the spine, so let your surgeon know.
Venous thrombosis (DVT - clotting of blood in your calf muscles) and pulmonary embolism are uncommon after an elective spine surgery, particularly when you are out of bed and walking within 24 hours after surgery. We use calf compressors and TED stockings to prevent the clotting of blood in legs; we do not routinely use medications. However, if you have had an episode of DVT in the past, let your surgeon know.
There are certain warning signs you should look for after surgery that may indicate a problem, such as excessive bleeding, redness or discharge from the wound, fever, weakness or numbness of the legs or problems urinating. If you notice any worrisome symptoms, notify your surgeon at once.
Are there any risks involved in disc surgery?
This is a brief overview and does not contain all the known facts about your condition and the surgery. Feel free to seek any clarifications from your surgeon and his or her team. It is important for you to obtain a clear understanding of your condition, the surgery and the potential risks and benefits before you sign the consent form.
Posterior Cervical Spine Surgery
Anatomy of the spine
The spine consists of 33 bony blocks called vertebrae stacked one above the other with a soft intervertebral disc between each pair of vertebrae. The intervertebral disc consists of a soft jelly-like substance called the nucleus pulposus in the centre, which is surrounded by multiple layers of collagen called the annulus fibrosis (like an onion). The disc connects and allows movement between the vertebrae and acts as a shock absorber for the spine. The vertebrae surround and protect the spinal cord and nerve roots.
The neck, also called the cervical spine, consists of seven vertebrae with an intervertebral disc in-between each pair of vertebrae.
Who needs a posterior cervical (neck) spine surgery?
- When the problem causing symptoms is located in the posterior aspect of the spine;
- when the compression on the spinal cord is from the posterior aspect;
- when the cervical spine is excessively mobile and unstable; or
- in association with an anterior procedure to provide additional stability or to achieve additional decompression.
The compression can be on the nerves going to the arms or on the spinal cord. Compression of the nerves in the neck can cause pain radiating down the arm and forearm with numbness, pins and needles, and muscular weakness in the affected limb. When the compression is on the spinal cord (myelopathy), it can cause difficulty in walking, clumsiness of the hands and problems with passing urine. The presence and severity of these symptoms vary from person to person. Pain in the neck could arise from numerous structures. Degeneration of the intervertebral disc and arthritis of the facet joints are the common causes of neck pain.
Who needs surgery?
Surgery is reserved for those with:
- No relief of pain with the non-operative forms of treatment;
- Increasing numbness and weakness in the arms and hands;
- Or the presence of myelopathy indicates the need for early surgery.
After assessing your symptoms, examining your spine, and studying your x-rays and scans, the surgeon will decide whether you need a posterior spinal decompression, a spinal fusion or a combination of both.
About the surgery
Anaesthesia: The surgery is usually performed under general anaesthesia, with the patient lying on the tummy. Occasionally, a frame is attached to the skull after anaesthesia, to maintain the position of the head during surgery.
Procedure: The surgeon makes a 5-15cm incision in the skin on the back of the neck. The spine is exposed by retracting the muscles. Depending on the plan, a decompression, a fusion or a combination of both is performed. A decompression is performed by removing one or more bony laminae and any other structure overlying the spinal cord. A fusion is performed by inserting screws into the bones over the back of the spine and connecting the screws with rods. Occasionally, a combination of a decompression and a fusion is performed. At the end of the surgery a drain tube is inserted to remove the blood that collects at the surgical site.
Skin sutures: Dissolvable sutures are used to close the skin. These will dissolve as your wound heals, however, the ends of the suture on either end of the incision will need to be cut on your first visit to the surgeon's office (7-10 days after surgery).
After the surgery
In the recovery room: Following surgery, you will be transferred to the recovery room and may feel some pain at the operated site when you wake up. A patient controlled analgesia (PCA) pump will be provided, which releases a small dose of pain medication every time you press the button thereby putting you in control of your pain. You will be given intravenous fluids to keep you hydrated and a urinary catheter will empty your bladder. A neck collar will be provided to prevent excessive neck movements and to keep you comfortable. When the medical staff in the recovery room is confident that you are comfortable, you will be transferred to your room.
In the ward: You will be allowed to drink sips of fluids after surgery and gradually progress to a full diet. The day after surgery, the drain tube, urinary catheter and pain pump will be removed and you will be encouraged to walk wearing a brace to support your spine. You will stay in the hospital for 1-3 days and your surgeon will decide when you can go home safely.
Are there any risks involved in disc surgery?
All surgical procedures are associated with a risk of complications and all risks should be discussed with your surgeon. The risks may be associated with the anaesthesia given or the surgical procedure. Surgical complications can include bleeding, infection, spinal fluid leak, injury to the veins and arteries near the spine or injury to the nerve tissue of the spine or its surrounding protective layer
Injury to the spinal cord or the nerves may occur during surgery and can result in complete paralysis of all four limbs or paralysis of certain muscles in the arms or legs with loss of normal sensation. Loss of bowel and bladder control can also occur following injury to the nerves. An injury to the covering layers of the nerves (dura) can result in a leak of spinal fluid and this may occasionally require a repeat surgery. Great care is taken to ensure the accurate placement of the screws including the use of intra-operative fluoroscopy (x-rays).
Although antibiotics are given before and after surgery, there is a 1-5% incidence of wound infection. Superficial mild infections can be treated with antibiotics, while deep infections may require a wound wash-out under anaesthesia. If you have had an infection in any other region (urinary bladder, chest and skin) immediately prior to surgery, you may be at a higher risk of post-operative infection in the spine, so let your surgeon know.
Venous thrombosis (DVT - clotting of blood in your calf muscles) and pulmonary embolism are uncommon after an elective spine surgery, particularly when you are out of bed and walking within 24 hours after surgery. We use calf compressors and TED stockings to prevent the clotting of blood in legs; we do not routinely use medications. However, if you have had an episode of DVT in the past, let your surgeon know.
There are certain warning signs you should look for after surgery that may indicate a problem, such as excessive bleeding, redness or discharge from the wound, fever, weakness or numbness of the legs or problems urinating. If you notice any worrisome symptoms, notify your surgeon at once.
Talk to your surgeon
This is a brief overview and does not contain all the known facts about your condition and the surgery. Feel free to seek any clarifications from your surgeon and his or her team. It is important for you to obtain a clear understanding of your condition, the surgery and the potential risks and benefits before you sign the consent form.
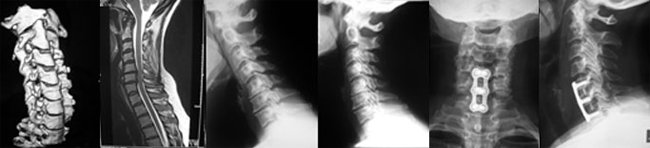
Spinal Deformity Surgery
What is the cause of a spinal deformity?
Scoliosis (abnormal sideward bending of the spine) and kyphosis (abnormal forward bending of the spine) can result from numerous causes. In a majority of adolescents, the exact cause is unknown (idiopathic) and in others it can be caused by congenital vertebral anomalies or as a manifestation of some other disease (eg neurofibromatosis, paralytic disorders etc). In adults, spinal deformity can be due to degenerative conditions, previous spinal surgery or even childhood deformities that have persisted. Some of these deformities can progress and need treatment.
When is surgery indicated for a spinal deformity?
In adolescents and children, surgery is indicated when curve progressive occurs or is anticipated, or to correct a cosmetic deformity that is unacceptable to the patient. In adults, pain relief and improving function may be additional considerations.
What are the surgical options for the correction of spinal deformities?
There are a number of alternatives in spine deformity surgery:
- An anterior procedure (from the front through the chest wall or abdomen) removes discs and corrects the deformity and maintains the correction with rods and screws inserted into your vertebral bones.
- Posterior surgery (from the back) can also be performed using rods, screws and hooks to correct the deformity and fuse the spine.
- Occasionally, a combination of an anterior and posterior procedure is needed, which can be done in one or more stages. Bone may be taken from your pelvis to assist in the spinal fusion. Your surgeon will discuss these options with you and decide which option is best suited in each case. Your surgeon and clinical co-ordinator will explain the surgical procedure to you in detail with the help of models and diagrams. Do not hesitate to clarify all your doubts prior to surgery so that you have a better understanding of and realistic expectations for the surgical procedure. Since there are many surgical options for the correction of spinal deformities, the precise surgical procedures will not be detailed here.
After surgery
In the recovery room: Following surgery, you will usually be transferred to the Intensive Care Unit (ICU) and may feel some pain at the operated site when you wake up. A patient controlled analgesia (PCA) pump will be provided, which releases a small dose of pain medication every time you press the button thereby putting you in control of your pain. You will be given intravenous fluids to keep you hydrated and a urinary catheter will empty your bladder. You may have a drainage tube from your surgical site or from you chest to help prevent the collection of blood in these areas. You may remain in the ICU for 24-48 hours and will be transferred to your room in the ward when the surgical team is satisfied with your progress.
In the ward: You will be allowed to drink sips of fluids after surgery and gradually progress to a full diet. The drainage tube, urinary catheter and pain pump will be removed in 24-48 hours and you will be encouraged to walk around. You will stay in the hospital for 5-7 days and your surgeon will decide when you can go home depending on your wound healing, ambulation and pain status.
Pain relief: Medications will be provided to reduce your pain after surgery and for the first 2 to 3 weeks at home. However, if you have excessive pain while you are in the hospital, the attending nurses should be informed.
Are there any risks involved in disc surgery?
All surgical procedures are associated with a risk of complications and all risks should be discussed with your surgeon. The risks may be associated with the anaesthesia given or the surgical procedure. The surgical complications include bleeding, infection, spinal fluid leak, injury to the veins and arteries near the spine, or injury to the nerve tissue or its surrounding protective layer.
Injury to the nerves may occur during surgery, resulting in paralysis of certain muscles in the legs and loss of sensations. Loss of bowel and bladder control can also occur following nerve injury. An injury to the covering layers of the nerves (dura) can result in leakage of spinal fluid and may occasionally require a repeat surgery to control the leak.
Although antibiotics are given before and after surgery, there is a 1-5% incidence of wound infection. Superficial infections can be treated with antibiotics, while deep infections may require a wound wash-out under anaesthesia. If you have had an infection in any other region (urinary bladder, chest and skin) immediately prior to surgery, you may be at a higher risk of post-operative infection in the spine, so let your surgeon know.
Venous thrombosis (DVT - clotting of blood in your calf muscles) and pulmonary embolism are uncommon after an elective spine surgery particularly when you are out of bed and walking within 24 hours after surgery. We use calf compressors and TED stockings to prevent the clotting of blood in legs, although we do not routinely use medications. However, if you have had an episode of DVT in the past, let your surgeon know.
The insertion of the screws can potentially cause nerve injury, resulting in weakness and abnormal sensations in the legs. Great care is taken to ensure the accurate placement of the screws, including the use of intra-operative fluoroscopy (x-rays). Correction of the deformity can also cause stretching of the nerves and spinal cord and may result in nerve injuries.
Another potential risk is that the fusion may not become solid, resulting in non-union, or pseudarthrosis. This may require a repeat surgery after a few months to supplement the bone graft to obtain a solid bony fusion.
There are certain warning signs you should look for after surgery that may indicate a problem, such as excessive bleeding, redness or discharge from the wound, fever, weakness or numbness of the legs or problems urinating. If you notice any worrisome symptoms, notify your surgeon at once.
Talk to your surgeon
This is a brief overview and does not include all the known facts about your condition and the surgery. Feel free to seek any clarifications from your surgeon and his or her team. It is important for you to obtain a clear understanding of the surgery and potential risks and benefits before you sign the consent form.
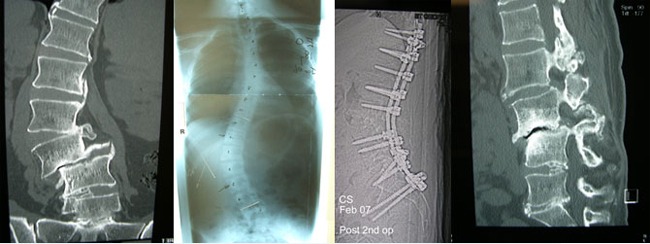
Lumbar Decompression and Fusion
Anatomy of the spine.
The spine consists of 33 small bones called vertebrae stacked one above the other with a soft intervertebral disc between each pair of vertebrae. The intervertebral disc consists of a soft jelly-like substance called the nucleus pulposus in the center, which is surrounded by multiple layers of collagen called the annulus fibrosis (like an onion). The disc connects and allows movement between vertebrae and acts as a shock absorber of the spine. The vertebrae surround and protect the spinal cord and nerve roots.
What does posterior spinal decompression mean?
Compression on the nerve roots exiting from the spinal canal can cause leg pain. A posterior spinal decompression includes either a partial (laminotomy) or complete (laminectomy) removal of the lamina along with the removal of the ligaments and new bone (osteophytes) that are compressing the nerve roots. The lamina is the bony portion of the vertebra that lies behind the spinal cord.
Spinal decompression is performed to relieve the compression on the nerves. The surgery is effective for the relief of the leg pain; however, weakness, numbness and pins and needles in the legs (if present) may take a few months to resolve and occasionally may not resolve completely, depending on the duration of symptoms.
What does spinal fusion mean?
Wear and tear (degeneration) of the spine can cause a loss of normal spinal alignment, excessive movement between vertebrae and arthritis of the spinal joints, all of which can cause low back pain. This can be treated by spinal fusion, where bone graft substitutes (VITOSS and OP-1) are placed around the vertebrae to form new bone connecting adjacent vertebrae so that they behave and move as one block.
The fusion is supplemented with rods (or plates) and screws to provide immediate stability. The screws are made of either titanium or stainless steel and are well tolerated by the body.
Which surgery will you need?
After assessing your symptoms, examining your spine and studying your x-rays and scans, the surgeon will decide whether you need a posterior spinal decompression, a spinal fusion or a combination of both.
About the surgery
Anaesthesia: The surgery is usually performed under general anaesthesia, with the patient lying face down.
Procedure: The surgeon makes a 5-10 cm incision in the skin over the affected area of the spine. The muscle is detached from the bone to expose the laminae, which are the portion of the bony vertebrae that lies behind the spinal cord. A portion of the lamina is removed (laminotomy) along with the surrounding ligaments to expose the compressed nerve roots. Occasionally, the whole lamina (laminectomy) is removed. The ligaments, intervertebral disc and new bone (osteophytes) that are pressing on the nerve roots are removed. This procedure is called a spinal decompression. Next, the surgeon may decide to fuse your spine using screws connected with rods or plates. A bone graft substitute (VITOSS and OP-1) is placed across the joints and bone at the back of the vertebrae to allow new bone to form (over 3-6 months) between the two adjacent vertebrae so that they now start behaving as one block. A drain tube removes the blood that collects at the surgical site. Skin sutures: Dissolvable sutures are used to close the skin. These will dissolve as your wound heals, however, the ends of the suture on either end of the incision will need to be cut on your first visit to the surgeon's office (7-10 days after surgery).
After surgery
In the recovery room: Following surgery, you will be transferred to the recovery room and may feel some pain at the operated site when you wake up. A patient controlled analgesia (PCA) pump will be provided, which releases a small dose of pain medication every time you press the button thereby putting you in control of your pain. You will be given intravenous fluids to keep you hydrated and a urinary catheter will empty your bladder. When the medical staff in the recovery room are confident that you are comfortable, you will be transferred to your room.
In the ward: You will be allowed to drink sips of fluids after surgery and gradually progress to a full diet. The day after surgery, the drain tube, urinary catheter and pain pump will be removed and you will be encouraged to walk wearing a brace to support your spine. You will stay in the hospital for 1-3 days and your surgeon will decide when you can go home.
Pain relief: Although we expect that you will be in pain or discomfort, we recommend that you take regular pain relief following surgery. Medications will be provided to reduce your pain after surgery and at home for the first 1-2 weeks. If pain persists after discharge please seek advice from Spine Service or your General Practitioner.
Skin sutures: Dissolvable sutures are most often used to close the skin. These will dissolve as your wound heals, however, the tip of the suture on either end of the incision will need to be cut on your first visit to the surgeon's office 7-10 days after surgery.
What to expect following surgery
Pain: You will feel discomfort and pain at the operative site immediately after surgery. You will be given pain medications; however, the soreness and stiffness in your back and/or limbs will continue for some time. Please ensure you take regular pain relief.
Tingling / Numbness: A degree of tingling and/or numbness in your limbs may be experienced after surgery and may take some time to subside.
Drains: Some patients may return to the ward with a drain tube near the surgical site to help prevent any collection of fluid at the operation site. The drain is usually removed in 24 to 48 hours.
Drips: You will have a small plastic needle (cannula) to receive fluids and antibiotics during and after surgery. The cannula will be removed when you are drinking sufficient fluids and after the doctor has stopped the prescribed antibiotics.
Catheter: A catheter will be inserted into your bladder under anaesthesia to drain you bladder during and immediately after surgery. This catheter will keep you comfortable, so you will not have to get out of bed to go to the toilet on the first day. The catheter is usually removed the day after surgery.
Calf compressors: Following your surgery, you will have inflatable compressors on your calves to reduce the risk of deep vein thrombosis (DVT). You may also be given a pair of anti-thrombotic stockings.
Coping with the Blues: It is not uncommon for patients to feel a little depressed or emotional after your surgery. The doctors and nurses will help you through this vulnerable phase.
Diet: You will be Nil by Mouth initially allowed only sips of fluid and crushed ice to suck. Once bowel sounds are present, you will start on a post-operative diet and gradually increase to a full diet. To avoid constipation, you should include plenty of roughage, cereals, fruit & vegetables in your diet. You should also aim to drink 2-3 litres of fluid daily.
Bowels: It is common not to have bowel movements for the first few days. Once you have started on a full diet, you will be given medications to help with bowel movements.
Are there any risks associated with this surgery?
All surgical procedures are associated with a risk of complications and all risks should be discussed with your surgeon. The risks may be associated with the anaesthesia given or the surgical procedure. Surgical complications can include bleeding, infection, spinal fluid leak, injury to the veins and arteries near the spine or injury to the nerve tissue or its surrounding protective layer.
Injury to the nerves may occur during surgery, resulting in paralysis of certain muscles in the legs and loss of sensations. Loss of bowel and bladder control can also occur following nerve injury. An injury to the covering layers of the nerves (dura) can result in leakage of spinal fluid and may occasionally require a repeat surgery to control the leak.
Although antibiotics are given before and after surgery, there is a 1-5% incidence of wound infection. Superficial infections can be treated with antibiotics, while deep infections may require a wound wash-out under anaesthesia. If you have had an infection in any other region (urinary bladder, chest and skin) immediately prior to surgery, you may be at a higher risk of post-operative infection in the spine, so let your surgeon know.
Venous thrombosis (DVT: clotting of blood in your calf muscles) and pulmonary embolism are uncommon after an elective spine surgery, particularly when you are out of bed and walking within 24 hours after surgery. We use calf compressors and TED stockings to prevent the clotting of blood in legs; we do not routinely use medications. However, if you have had an episode of DVT in the past, let your surgeon know.
The insertion of the screws can potentially cause nerve injury resulting in weakness and abnormal sensations in the legs. Great care is taken to ensure the accurate placement of the screws including the use of intra-operative fluoroscopy (x-rays).
There are certain warning signs you should look for after surgery that may indicate a problem, such as excessive bleeding, redness or discharge from the wound, fever, weakness or numbness of the legs or problems urinating. If you notice any worrisome symptoms, notify your surgeon at once.
Talk to your surgeon
This a brief overview and does not contain all the known facts about your condition and the surgery. Feel free to seek any clarifications from your surgeon and his or her team. It is important for you to obtain a clear understanding of your condition, the surgery, the potential risks and benefits before you sign the consent form.
Lumbar Discectomy
Anatomy of the Spine
The spine consists of 33 bony blocks called vertebrae stacked one above the other with a soft intervertebral disc between each pair of vertebrae. The intervertebral disc consists of a soft jelly-like substance called the nucleus pulposus in the center, which is surrounded by multiple layers of collagen called the annulus fibrosis (like an onion). The disc connects and allows movement between vertebrae and acts as a shock absorber for the spine. The vertebrae surround and protect the spinal cord and nerve roots.
What is a disc prolapse?
This is also referred to as a slipped disc or disc herniation. The soft central portion of the disc (nucleus pulposus) tears through the surrounding layers (annulus pulposus) and compress nerves extending from the spinal cord. This compression on the nerves causes pain in the legs (sciatica), which increases on bending forwards, coughing and sneezing. Numbness, pins and needles, and muscular weakness in the legs may also be present. Rarely, there can be difficulty in passing urine and stools. The presence and severity of these symptoms vary from person to person.
About the surgery
Anaesthesia: The surgery is usually performed under a general anaesthetic, with the patient lying face down.
Procedure: The surgeon makes a 2.5-5cm incision in the skin over the affected area of the spine. The muscle is detached from the bone to reveal the laminae, which are the portion of the bony vertebrae that lies behind the spinal cord. A portion of the lamina is removed (laminotomy) along with the surrounding ligaments to expose the prolapsed disc. Occasionally, the whole lamina has to be removed (laminectomy) to access the disc. The bulging parts of the intervertebral disc, along with adjacent loose disc fragments, are removed. The resultant space is not filled with any material but is eventually filled with scar (fibrous) tissue. A drain tube removes the blood that collects at the surgical site.
Skin sutures: Dissolvable sutures are used to close the skin. These will dissolve as your wound heals, however, the ends of the suture on either end of the incision will need to be cut on your first visit to the surgeon's office (7-10 days after surgery).
After surgery
In the recovery room: Following surgery, you will be transferred to the recovery room and may feel some pain at the operated site when you wake up. A patient controlled analgesia (PCA) pump will be provided which releases a small dose of pain medication every time you press the button thereby putting you in control of your pain. You will be given intravenous fluids to keep you hydrated and a urinary catheter will empty your bladder. When the medical staff in the recovery room are confident that you are comfortable, you will be transferred to your room.
In the ward: You will be allowed to drink sips of fluids after surgery and gradually progress to a full diet. The day after surgery, the drain tube, urinary catheter and pain pump will be removed and you will be encouraged to walk wearing a brace to support your spine. You will stay in the hospital for 1-3 days and your surgeon will decide when you can go home.
Pain relief: Medications will be provided to reduce your pain after surgery and at home for the first 1-2 weeks. However, if you have excessive pain while you are in the hospital, the attending nurses should be informed.
Results after surgery
Eighty to eighty-five per cent of patients have a good outcome after a lumbar disc surgery. While there is considerable relief of the leg pain after surgery, the pins and needles, numbness and weakness in the legs may take 3-6 months to resolve, depending on the duration and severity of nerve compression. If the compression has occurred for a long period, complete resolution of the abnormal sensations and weakness may not occur. There is also a 5-10 % incidence of recurrent disc herniation at the same level after surgery.
Are there any risks involved in disc surgery?
All surgical procedures are associated with a risk of complications and all risks should be discussed with your surgeon. The risks may be associated with the anaesthesia given or the surgical procedure. Surgical complications can include bleeding, infection, spinal fluid leak, injury to the veins and arteries near the spine or injury to the nerve tissue or its surrounding protective layer.
Injury to the nerves may occur during surgery resulting in paralysis of certain muscles in the legs and loss of sensations. Loss of bowel and bladder control can also occur following nerve injury. An injury to the covering layers of the nerves (dura) can result in leakage of spinal fluid and may occasionally require a repeat surgery to control the leak.
Although antibiotics are given before and after surgery, there is a 1-5% incidence of wound infection. Superficial infections can be treated with antibiotics, while deep infections may require a wound wash-out under anaesthesia. If you have had an infection in any other region (urinary bladder, chest and skin) immediately prior to surgery, you may be at a higher risk of post-operative infection in the spine, so let your surgeon know.
Venous thrombosis (DVT: clotting of blood in your calf muscles) and pulmonary embolism are uncommon after an elective spine surgery, particularly when you are out of bed and walking within 24 hours after surgery. We use calf compressors and TED stockings to prevent the clotting of blood in legs; we do not routinely use medications. However, if you have had an episode of DVT in the past, let your surgeon know.
There are certain warning signs you should look for after surgery that may indicate a problem, such as excessive bleeding, redness or discharge from the wound, fever, weakness or numbness of the legs or problems urinating. If you notice any worrisome symptoms, notify your surgeon at once.
Talk to your surgeon
This is a brief overview and does not contain all the known facts about your condition and the surgery. Feel free to seek any clarifications from your surgeon and his or her team. It is important for you to obtain a clear understanding of the surgery and potential risks and benefits before you sign the consent form.
Surgical Risks
What are the risks involved in spinal surgery?
All surgical procedures are associated with a risk of complications and all risks should be discussed with your surgeon. The risks may be associated with the anaesthesia or the surgical procedure. Surgical complications can include bleeding, infection, spinal fluid leak, injury to the veins and arteries near the spine or injury to the spine's nerve tissue or its surrounding protective layer
Injury to the spinal cord or the nerves may occur during surgery and can result in complete paralysis of all four limbs or paralysis of certain muscles in the arms or legs, with loss of normal sensation. Loss of bowel and bladder control can also occur following injury to the nerves. An injury to the covering layers of the nerves (dura) can result in a leak of spinal fluid and this may occasionally require a repeat surgery. Great care is taken to ensure the accurate placement of the screws, including the use of intra-operative fluoroscopy (x-rays).
Although antibiotics are given before and after surgery, there is a 1% to 5% incidence of wound infection. Superficial mild infections can be treated with antibiotics, while deep infections may require a wound wash-out under anaesthesia. If you have had an infection in any other region (urinary bladder, chest and skin) immediately prior to surgery, you may be at a higher risk of post-operative infection in the spine, so let your surgeon know.
Venous thrombosis (DVT - clotting of blood in your calf muscles) and pulmonary embolism are uncommon following an elective spine surgery, particularly when you are out of bed and walking within 24 hours after surgery. We use calf compressors and TED stockings to prevent the clotting of blood in legs; we do not routinely use medications. However, if you have had an episode of DVT in the past, let your surgeon know.
There are certain warning signs you should look for after surgery that may indicate a problem, such as excessive bleeding, redness or discharge from the wound, fever, weakness or numbness of the legs, or problems urinating. If you notice any worrisome symptoms, notify your surgeon or his office at once..
Talk to your surgeon
This is a brief overview and does not include all the known facts about your condition and the surgery. Feel free to seek any clarifications from your surgeon and his or her team. It is important for you to obtain a clear understanding of your condition, the surgery and the potential risks and benefits before you sign the consent form.
FAQ's
Will I need a blood transfusion?
Although some blood loss occurs during surgery, a blood transfusion is not generally required. More extensive surgeries may occasionally require a blood transfusion.
How long will I stay in hospital?
The length of your stay in the hospital will depend on the surgical procedure that you have had and can vary from an overnight stay to a week. It will also depend on how your wound is healing. You will be given a rough idea regarding the length of your stay during the pre-surgical education session. However, your surgeon will make a final decision after the operation.
When can I walk?
You will usually be encouraged to begin walking the morning after surgery.
Do I have to wear a back/neck brace?
Yes, you will be required to wear your brace when sitting, standing and walking after surgery. Your physiotherapist will wean you off as appropriate.
When can I have a shower after my surgery?
You can have a shower the day after your surgery. If your dressing gets wet, a new one can be applied.
When do I see my doctor after my surgery?
During your pre-surgical education session, the clinical co-ordinator will make an advance appointment for you to visit the rooms after you have been discharged from the hospital. This date can be changed depending on the length of your hospital stay.
Do I have stitches to come out?
The wound is usually closed with dissolvable sutures under the skin and these do not need to be removed. Metallic staples or non-dissolvable sutures, if used, will need removal. On your first appointment (10 days post-op) the surgical wound will be examined and the sutures/staples will be removed.
Do I need to attend physiotherapy sessions?
Following surgery a physiotherapy programme will be started to retrain you to maintain good posture and teach you the correct way of moving your spine.
Is there a certain position that I should sleep in at night?
The most important thing is for you to be comfortable. Some people find it comfortable to sleep with a pillow between their legs or under their thighs.
When is it safe to engage in sexual relations?
This is a very personal domain and is left up to you; whenever you think that you and your partner are ready. Clinically, a two-week period is recommended, provided you are the less active partner.
How long should I wait before driving a car?
The recommendation is to wait 3-4 weeks before driving a car. This may vary depending on your surgery and your progression during rehabilitation.
When can I go back to work?
This is assessed on patient-to-patient bases. If you have a physical occupation, it may take up to 3-6 months. With a sedate occupation, you could be back at work as soon as 3 weeks. Do not commence work until you speak to your doctor and physiotherapist.
When is it safe to bend and/or lift items heavier than a bag of sugar?
During the post-surgical physiotherapy sessions, you will be taught the correct way to bend and lift. Bending from the hips is fine if carried out in a controlled manner, but avoid heavy lifting objects (more than 3kg) till your physiotherapy commences.